Case Studies
Type 3 multiple autoimmune syndrome: A case report
Jayashankar CA1* a, Bhanu Prakash2 a, DS Somasekar3 a, Venkata Bharatkumar4 a, Laxmish Naik5 a, Riddhima Srivastava5 a
Author Affiliations
1Associate Professor, Department of General Medicine
2Professor, Department of Dermatology
3Professor and Head, Department of General Medicine
4Associate Professor Department of Biochemistry
5Post graduate, Department of General Medicine*
aVydehi Institute of Medical Sciences and Research Centre, White field, Bangalore-560066, Karnataka, India.
Correspondence: Dr. Jayashankar CA
IJRCI. 2014;2(1):CS2.
Received: 26 March 2014, Accepted: 9 April 2014, Published: 23 April 2014
© IJRCI
Abstract
Multiple autoimmune syndrome (MAS) is a distinctive subgroup of autoimmune disorders characterized by the co-occurrence of three or more autoimmune diseases in a single patient. We report here a case of 31-year-old male with co-existence of three autoimmune diseases, namely, autoimmune hypothyroidism, pernicious anemia and vitiligo, which has been finally diagnosed as MAS.
Introduction
Multiple autoimmune syndrome (MAS) is defined as the co-existence of at least three autoimmune diseases in the same patient.1 Vitiligo has been identified as an important dermatological disease associated with MAS. As per the literature evidence, vitiligo is strongly associated with autoimmune hypothyroidism and pernicious anemia with prevalence of 12 and 1.3% respectively.2
Case report
A 31-year-old unmarried male presented to our hospital with a history of insidious onset of easy fatigability since 4 years. There was no history of breathlessness, palpitations, chest pain, syncopal episodes, cough, melena, hematemesis, hemoptysis or hematuria. The patient had been suffering from generalized vitiligo since past 4 years and was on regular treatment of potent topical steroid and tacrolimus 0.03%. The patient was also on oral thyroxine 100 mcgs/day since 3 years for hypothyroidism. He did not have motor weakness, joint pain, swelling of joints, hemorrhagic skin lesions, jaundice, chronic diarrhea, and dryness of tongue or eyes. The patient was not a known case of hypertension, diabetes mellitus or heart disease. Family history revealed that his cousin and nephew had been suffering from vitiligo.
General physical examination revealed that the patient was moderately built, conscious, well oriented, and poorly nourished with normal vital parameters. He was pale and had no edema, clubbing, cyanosis, lymphadenopathy or goiter. Jugular venous pressure was normal. Examination of skin (Fig 1) revealed the presence of multiple, polysized, irregular, asymmetrical, dry, well-defined hypo to de-pigmented patches over the dorsum of the hands, feet, lower back, and on the anterior aspect of neck. Clinical examination of respiratory, abdomen, nervous system and locomotor systems were unremarkable. The significant findings of lab investigations are given in table 1.
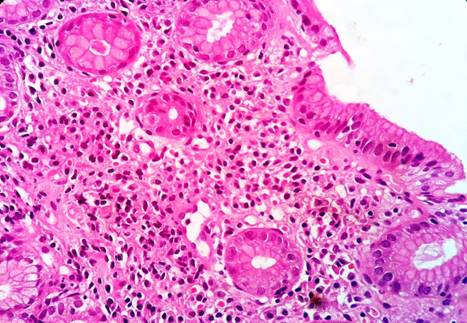
Peripheral blood smear showed dimorphic anemia of severe degree. Random blood glucose, blood urea, serum creatinine, serum sodium, potassium, chloride, calcium, phosphorous and liver function tests were normal. Urine, stool, and bone marrow examinations were normal. Auscultation of heart revealed short systolic murmur of grade 2/6 in pulmonary area. Electrocardiogram indicated sinus tachycardia of 109/min. Chest X-ray posterior anterior view, 2-D echocardiogram and ultrasonographic (USG) examination of abdomen and pelvis were normal. USG of thyroid glands showed diffuse increase in echo-texture. Upper GI endoscopy revealed mild thinning of mucosal folds in fundus of stomach. Histopathological examination of gastric biopsy revealed features of chronic atrophic gastritis (Fig 2 and Fig 3). Based on the aforementioned lab findings and clinical evaluations, which indicated the co-existence of vitiligo, autoimmune hypothyroidism and pernicious anemia with atropic gastritis, the diagnosis was concluded as type 3 MAS.
1: Results of lab investigations
Fig 1: De-pigmented patches over the dorsum of the hands

Fig 2: Atrophic mucosal surface with underlying glands in cross section (H&E, x100)
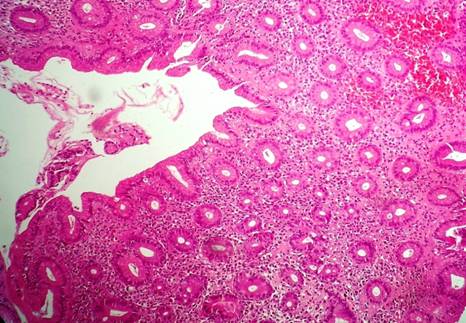
Fig 3: Bland mucosal epithelium lining surface and glands with lymphocytes
in lamina propria (H&E, x400)
The patient was treated with 2 units of packed cells transfusion, IM vitamin B12 injection, and oral thyroxine 125 mcg/day daily. Further follow-up showed significant symptomatic improvement and increase in Hb count (8.1 gm%).
Discussion
According to the literature evidence, patients suffering from single autoimmune disorder are at 25% increased risk of developing another autoimmune disorder.3 MAS is an unusual condition with constellation of at least 3 autoimmune disorders. MAS is classified into type 1, type 2, and type 3 based on the prevalence of their associations with one another (Table 2).3
2: Classification of MAS
Although the role of various genetic, infectious, immunological and psychological factors has been implicated in the development of MAS, the exact etiopathogenesis is not known.4 HLA-B8, DR3 and DR5 are the important genetic factors implicated in the etiopathogenesis of type 3 MAS.3
The present patient was suffering from vitiligo and hypothyroidism along with the features of severe anemia. On evaluation, he was diagnosed to have pernicious anemia with atropic gastritis and autoimmune hypothyroidism. Genetic studies were not done in the present case due to the unavailability of resources in our hospital.
The differential diagnoses considered in the present case are autoimmune polyendocrine syndrome type 3B and type 3C. Autoimmune polyendocrine syndrome (APES) type 3B comprises of autoimmune thyroid disease, pernicious anemia, celiac disease, chronic inflammatory bowel diseases, autoimmune hepatitis, primary biliary cirrhosis and primary sclerosing cholangitis, but not vitiligo.5 Type 3C includes autoimmune thyroid disease, vitiligo, alopecia, autoimmune thrombocytopenia, autoimmune hemolytic anemia, antiphospholipid antibody syndrome, myasthenia gravis, stiff-man syndrome and multiple sclerosis but no pernicious anemia.5 Hence, the final diagnosis is concluded as MAS and not APES.
Conclusion
Early diagnosis of individual components of MAS and commencement of treatment is essential to curb morbidity and mortality associated with MAS. The case study also warrants the need for continued surveillance of predisposed patients for MAS. In any patient with vitiligo and anemia, pernicious anemia as an autoimmune cause for anemia should be considered.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. Humbert P, Dupond JL. Multiple autoimmune syndromes. Ann Med Interne. 1988;139(3):159-68.
2. Sawicki J, Siddha S, Rosen C. Vitiligo and associated autoimmune disease: retrospective review of 300 patients. J Cutan Med Surg. 2012;16(4):261-6.
3. Mohan MP, Ramesh TC. Multiple autoimmune syndrome. Indian J Dermatol Venereol Leprol. 2003; 69(4): 298-9.
4. Cojocaru M, Cojocaru IM, Silosi I. Multiple autoimmune syndrome. Maedica (Buchar). 2010 Apr;5(2):132–4.
5. Betterle C, Zanchetta R. Update on autoimmune polyendocrine syndromes (APS). Acta Biomed. 2003; 74(1): 9-33.