Case Studies
Rheumatoid arthritis with ANCA associated vasculitis
Vikram Haridas1, Kiran Haridas2
Author Affiliations
1,2 Arthritis Super Speciality Center, Hubli, Karnataka, India
*Correspondence: Dr. Vikram Haridas
haridasvikram@yahoo.co.in
IJRCI. 2018;6(1):CS7
Submitted: 23 August 2018, Accepted: 30 November 2018,
Published: 7 december 2018
© IJRCI
Abstract
Antineutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) are rarely associated with autoimmune diseases. The present report describes an uncommon case of a 50-year old women with the co-occurrence of antineutrophil cytoplasmic antibody associated vasculitis with rheumatoid arthritis. The patient was treated with steroids and cyclophosamide and achieved complete recovery of the lesions, following 4-weeks of treatment.
Keywords: Rheumatoid arthritis, ANCA, ANCA associated vasculitis, autoimmune diseases
Introduction
Antineutrophil cytoplasmic antibody associated vasculitis are rare autoimmune diseases, characterized by inflammation of small and medium sized blood vessels.1 AAV is rarely associated with immune mediated diseases such as systemic lupus erythematosus, scleroderma, membranous glomerulonephritis and anti-glomerular basement membrane disease.2 Recent studies have reported the development of AAV in patients with rheumatoid arthritis.2 The present study discusses an uncommon case of AAV in a 50-year old patient with RA.
Case Report
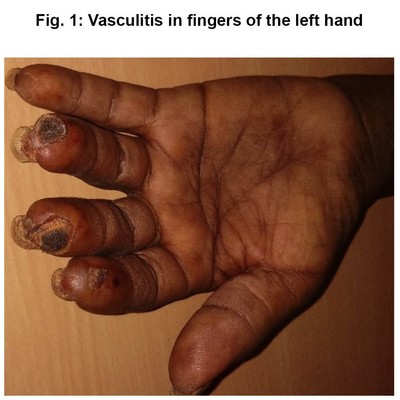
A 50-year-old female presented to the outpatient department with sudden onset blackening of ring, index and middle finger of the left-hand (Fig. 1). The symptom was progressive with associated severe paresthesia throughout the hand. She was diagnosed with seropositive rheumatoid arthritis from two-years and was on methyl prednisolone (5 mg/day) and methotrexate (10 mg/week), for 6-months. The subject fulfilled the 2010 ACR EULAR criteria for RA. History of fever, chest pain, skin rashes, reduced urine output, trauma, sinusitis, cough and hemoptysis were absent in the patient.
The blood pressure, pulse and SpO2 of the patient was 160/90,100 and 99% respectively. Reduced pulse was noted in the radial and ulnar arteries of the left hand. Tenderness was noted in few joints of the hand with minimal swelling. The patient had normal cardiovascular function.
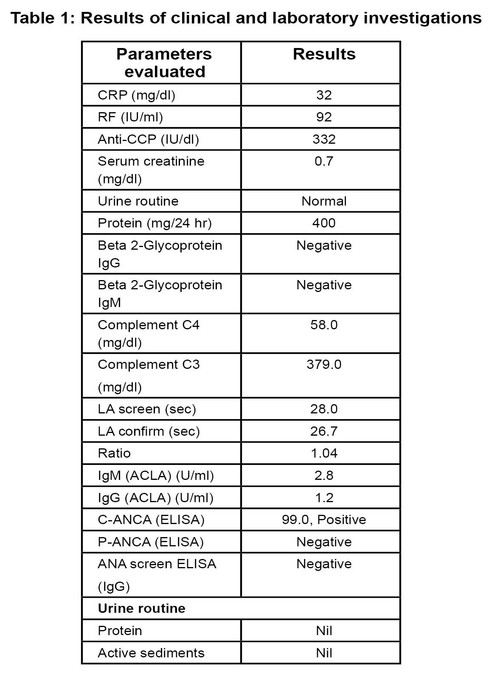
ANA and APLA workup of the patient was negative with highly positive C-ANCA (Table 1). Her chest X-ray was normal. The ultrasound scan of the abdomen showed normal kidneys, and the upper limb doppler revealed the presence of narrow lumen in the radial and ulnar arteries of the left hand, with decreased blood flow and spectral widening.
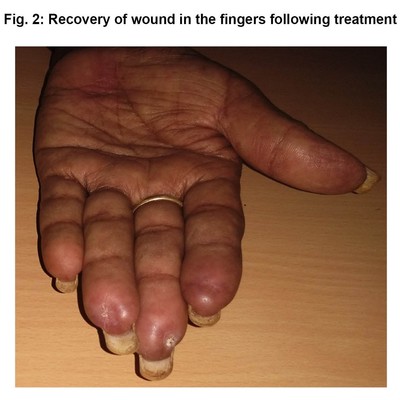
Based on the clinical and laboratory findings, the patient was diagnosed with ANCA associated vasculitis, concurrent with rheumatoid arthritis. She was prescribed steroids with Eurovas regimen and cyclophosamide at a dose of 500 mg/two weeks. Following six cycles of cyclophosamide treatment, the subject was maintained with azathioprine therapy. The patient acquired complete recovery of the lesion in the fingers, after 4-weeks of treatment (Fig. 2).
Fig. 1: Vasculitis in fingers of the left hand
Fig 2: Radiography showing constriction of soft tissue and thinning of underlying bones
Table 1: Results of clinical and laboratory investigations
Discussion
Active vasculitis associated with RA is a rare complication, affecting only about 1% of the patient population, and occurs in patients with longstanding RA and with severe joint deformities.3 Apart from classic presentation of rheumatic vasculitis, mononeuritis multiplex, other manifestations include weight loss, hepatomegaly, splenomegaly, ocular inflammation, pleuritis, pericarditis, and Felty’s syndrome.4 The involvement of kidney is less common in rheumatic vasculitis.5
ANCA associated vasculitis constitutes: microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA) or Wegener’s granulomatosis and eosinophilic granulomatosis with polyangiitis (EGPA) or Churg-Strauss syndrome, and occurs from the antineutrophil cytoplasmic antibody, directed towards myeloperoxidase (MPO) or proteinase 3 (PR3).6 Clinically, MPA mostly involves MPO-ANCA and GPA involves PR3-ANCA.6 The disease effects organs such as kidney, stomach, intestine, and lungs, and include clinical features such as fever, anemia, malaise, weight loss, synovitis and rash.7, 8
In the present patient, RA activity was less severe with minimal joint tenderness and swelling, and was of short duration. The ultrasound of the abdomen revealed only mild fatty liver and normal kidneys. Additionally, the cardiovascular function was normal. Hence the possibility of RA associated vasculitis was less likely. However, the patient had highly positive c-ANCA values, indicating associated GPA.
Renal involvement is a common manifestation in AAV. The highest frequency of renal involvement has been reported in MPA (upto 100%), followed by GPA (upto 70%) and EGPA.9, 10 Draibe and Salama (2015), based on a retrospective analysis concluded that renal involvement is a common manifestation among rheumatoid arthritis patients developing AAV.2 However, in the present patient renal involvement was absent.11
ANCA associated vasculitis typically involves capillaries, arterioles, venules and small vessels.12 Literature evidence suggests that the involvement of large and medium sized vessels in ANCA associated vasculitis has a lower prevalence.12 However, in the present patient, narrow lumen was noted in medium vessels such as the left hand radial and ulnar artery. There was no involvement of other small vessels for the patient, which is a classical presentation of the disease.
Over 35 cases of overlap between RA and AAV has been reported so far.2 The cohort study conducted by Draibe and Salama (2015) reported six cases of RA patients developing ANCA associated vasculitis in an average 10.5 years, following the diagnosis of RA.2 The study reported that the patients frequently presented with vasculitis renal manifestations and RF positivity, during AAV diagnosis. Similarly, previous studies have also reported function deformity in renal and RF positivity in majority of the cases. However, cases of overlapping RA and AAV with negative ANCA was also reported.2
The overlap of RA with AAV has been attributed to the presence of common genes, such as the PTPN22, found in both RA and AAV.13, 14 The study by Menegatti et al. (2009) suggested that genetic variation in uteroglobin and NF-kappaB2 are associated with the development of RA and ANCA associated vasculitis.15
AAV is treated with induction therapy, which uses a combination of cyclophosphamide and steroids, at high doses.16 Methotrexate and mycophenolate mofetil are considered for induction therapy in patients with no evidence of major organ disease.17 Maintenance therapy mostly involves the use of azathioprine. However, recent studies have demonstrated the superiority of rituximab over azathioprine.18 The commonly used drugs for the treatment of RA includes methotrexate, prednisolone, anti-TNFs and hydroxychloroquine. ANCA associated vasculitis are treated with drugs such as cyclophosphamide, glucocorticoids and rituximab.8
Conclusion
Although ANCA associated vasculitis is rare, they should be considered in RA patients without active disease.
Competing interests
The authors declare that they have no competing interest.
References
1. Lazarus B, John GT, O’Callaghan C, Ranganathan D. Recent advances in anti-neutrophil cytoplasmic antibody-associated vasculitis. Indian J Nephrol 2016;26(2):86–96.
2. Draibe J, Salama AD. Association of ANCA associated vasculitis and rheumatoid arthritis: a lesser recognized overlap syndrome. Springerplus [Internet]. 2015 [cited 2018 Aug 22];4:50. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315802/
3. Johns Hopkins Vasculitis Center. Rheumatoid Vasculitis [Internet]. Johns Hopkins Vasculitis Center. [cited 2018 Aug 22]. Available from: https://www.hopkinsvasculitis.org/types-vasculitis/rheumatoid-vasculitis/
4. Vollertsen RS, Conn DL. Vasculitis associated with rheumatoid arthritis. Rheum Dis Clin North Am 1990;16(2):445–61.
5. Bartels CM, Bridges AJ. Rheumatoid Vasculitis: Vanishing Menace or Target for New Treatments? Curr Rheumatol Rep 2010;12(6):414–9.
6. Kallenberg CGM. Pathogenesis of ANCA-associated vasculitides. Ann Rheum Dis 2011;70 Suppl 1:i59-63.
7. McKinney EF, Willcocks LC, Broecker V, Smith KGC. The immunopathology of ANCA-associated vasculitis. Semin Immunopathol 2014;36(4):461–78.
8. ANCA-associated vasculitis | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program [Internet]. [cited 2018 Aug 22]. Available from: https://rarediseases.info.nih.gov/diseases/13011/anca-associated-vasculitis
9. Sinico RA, Di Toma L, Radice A. Renal involvement in anti-neutrophil cytoplasmic autoantibody associated vasculitis. Autoimmun Rev 2013;12(4):477–82.
10. Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med 1997;337(21):1512–23.
11. Mansi IA, Opran A, Rosner F. ANCA-Associated Small-Vessel Vasculitis. Am Fam Physician 2002;65(8):1615-20.
12. Villacorta J, Díaz-Crespo F, Stanescu R, Fernandez-Juarez G. Large and Small vessel Severe Involvement in ANCA-Associated Vasculiitis. Journal of Vasculitis 2016;2(2):1–3.
13. Johansson M, Arlestig L, Hallmans G, Rantapää-Dahlqvist S. PTPN22 polymorphism and anti-cyclic citrullinated peptide antibodies in combination strongly predicts future onset of rheumatoid arthritis and has a specificity of 100% for the disease. Arthritis Res Ther 2006;8(1):R19.
14. Jagiello P, Aries P, Arning L, Wagenleiter SEN, Csernok E, Hellmich B, et al. The PTPN22 620W allele is a risk factor for Wegener’s granulomatosis. Arthritis Rheum 2005;52(12):4039–43.
15. Menegatti E, Davit A, Francica S, Berardi D, Rossi D, Baldovino S, et al. Genetic factors associated with rheumatoid arthritis and systemic vasculitis: Evaluation of a panel of polymorphisms. Dis Markers 2009;27(5):217–23.
16. 16. Fauci AS, Katz P, Haynes BF, Wolff SM. Cyclophosphamide therapy of severe systemic necrotizing vasculitis. N Engl J Med 1979;301(5):235–8.
17. Yates M, Watts R. ANCA-associated vasculitis. Clin Med (Lond) 2017;17(1):60–4.
18. Guillevin L, Pagnoux C, Karras A, Khouatra C, Aumaître O, Cohen P, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med 2014;371(19):1771–80.