Case Studies
Primary antiphospholipid syndrome presenting as gross communicating hydrocephalus
Dibya Ranjan Behera1*, Nand Kumar Singh2, Manoj Godara3
Author Affiliations
1 Junior resident, General Medicine, Institute of Medical Sciences (IMS), Banaras Hindu University (BHU), Varanasi, India
2 Professor of Medicine and Head Division of Rheumatology, Institute of Medical Sciences, BHU, India
3Junior resident, General Medicine, IMS, BHU, India
* Correspondence: Dr. Dibya Ranjan Behera
IJRCI. 2013;1(1):CS1
Received: 29 January 2013, Accepted: 15 February 2013, Published: 26 February 2013
© IJRCI
Abstract
Primary antiphospholipid syndrome (APS) presents with a wide variety of neurological syndromes. But, hydrocephalus is seen very rarely. We report a case of gross communicating hydrocephalus in a 20-year-old woman with primary APS presented with headache and blurring of vision, without any focal neurologic signs. Magnetic resonance venography revealed superior sagittal sinus and bilateral cortical vein thrombosis.
Introduction
Antiphosoholipid syndrome (APS) is a systemic autoimmune disorder characterized by recurrent venous or arterial thrombosis and/or fetal losses. The frequent neurological manifestations described in APS are cerebrovascular disease, dementia, chorea, epileptic seizures, headache, psychosis, transverse myelopathy, and multiple sclerosis-like presentations. Although idiopathic intracranial hypertension is not uncommon in primary APS, reports of hydrocephalus in primary APS are very rare. Till date, only two case studies have been reported: one in secondary APS (systemic lupus erythematosus with APS) and the other in primary APS.1, 2 So far, there has been no case report on gross communicating hydrocephalus in primary APS. We describe a case of gross communicating hydrocephalus in a 20-year-old woman with primary APS.
Case report
A 20-year-old unmarried female presented at the medicine outpatient department with complaints of headache since 8 months and blurring of vision since 6 months. The headache was global, persistent, and with increasing severity. It was also associated with disturbed sleep, frequent nausea, and vomiting. Two months after the development of headache, she noticed progressive blurring of vision in both the eyes. She denied any history of fever or focal neurological deficit including seizure, cranial nerve palsies or hemiparesis. There was no history suggestive of arterial or venous thrombotic event in past. The woman was nulliparous and without any bad obstetric history. She had no history of skin rash, arthralgia, alopecia, photosensitivity, or low grade fever.
She was normotensive and other general examinations were found to be normal. Additionally, no abnormal findings were noted during neurological examination and while measuring pupillary reactivity. However, a decrease in visual acuity (20/50) was noted and the fundoscopic examination revealed bilateral optic atrophy. Initial laboratory data revealed sedimentation rate of 23 mm/h, hemoglobin of 10.8 g/dl with normal indices, white blood count of 8.2x103/mm3, and platelet count of 370,000/mm3. Liver function and renal function tests were within normal limits. Urine routine and microscopy was unremarkable with absence of cells, casts, and bacteria. Chest radiography and ECG were normal. EEG revealed slowing of all cortical background rhythms. Cerebrospinal fluid (CSF) obtained through lumbar puncture was clear and colorless, and with protein and glucose levels of 20 mg/dl and 42 mg/dl respectively. Opening pressure of CSF noted in sitting posture was 700mm water (normal value 200-400mm water). CSF adenosine deaminase was within the normal limit. Microbial tests for CSF such as acid fast bacilli staining, PCR for tuberculosis, and test for fungal infection by India ink yielded negative results.
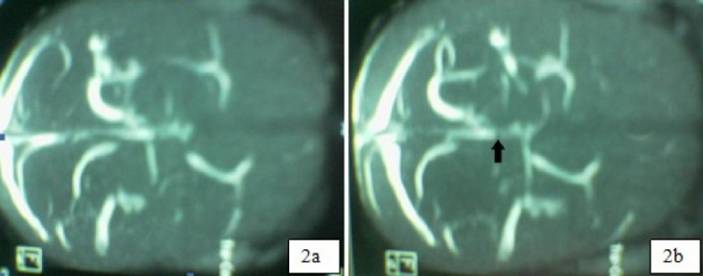
Anti-nuclear antibody and anti-double stranded DNA were within the normal limits. CT scan of brain revealed large dilated ventricles. Both lateral ventricles, and third and fourth ventricles were prominently dilated, and all cisterns of the posterior fossa and suprasellar cistern were also dilated (Figure 1a and 1b). All these findings suggested that the patient had gross communicating hydrocephalus. No neural parenchymal lesion or pathologic contrast enhancement was found in the CT scan. Contrast-enhanced magnetic resonance venography showed patchy filling defects in superior sagittal sinus and bilateral cortical veins, indicating the occurrence of thrombosis (Figure 2a and 2b).
Figure 1a and 1b: Gross communicating hydrocephalous in longitudinal (sagittal) (1a) and transverse sections (1b)
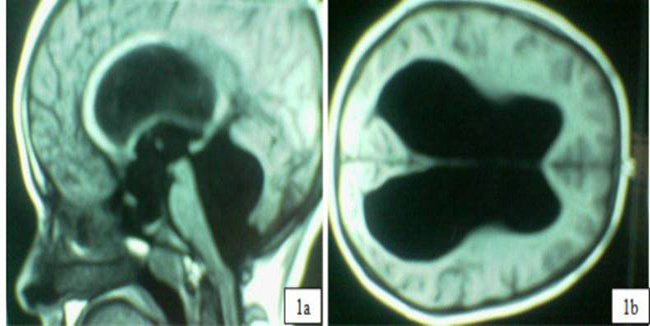
Figure 2a and 2b: MR venography showing patchy filling defect in superior sagittal sinus (arrow) and paucity of bilateral cortical veins
Abnormal increase in the levels of anticardiolipin (aCL) IgG antibody (81.6 GPLU/ml; normal <10 GPLU/ml), lupus anticoagulant (dRVVT-1.88; normal <1.3), and anti-β2-glycoprotien 1 IgM (68.00 U/ml; normal ≤20 MPLU/ml) was also reported. Based on the study results, a provisional diagnosis of primary APS with intracranial sinus and cortical vein thrombosis with gross communicating hydrocephalus was made. The occurrence of raised intracranial tension with secondary optic atrophy was also documented. Analysis conducted after 12 weeks also showed an increase in aCL IgG titre (38.2 GPLU/ml), and a positive lupus anticoagulant (dRVVT-1.45), thus confirming the diagnosis of primary APS according to the revised 2006 Sapporo classification criteria.3
The patient was initiated with low-molecular-weight heparin injection (LMWH; 0.4ml, s/c BD) along with oral warfarin 3mg/day to maintain the international normalized ratio between 2 to 3. The administration of LMWH was subsequently withdrawn. The patient also underwent shunting operations to circumvent the raised intracranial tension. Following the shunting operation and the anticoagulant therapy, a significant improvement in symptoms such as headache, vomiting, and blurred vision was noted. Follow-up conducted after 2 months showed a marked decrease in all the symptoms except for modest improvement in blurred vision (visual acquity-20/30).
Discussion
APS, an autoimmune disease characterized by arterial and/or venous thrombosis and bad obstetric outcome, is the most common acquired cause for thrombotic disorders. Antiphospholipid antibodies constitute a heterogeneous family of autoantibodies directed against membrane anionic phospholipids (aCL antibody, antiphosphatidylserine) or their associated plasma proteins, predominantly β-2 glycoprotein I.4
APS presents with a wide variety of neurological disorders such as cerebrovascular disease, dementia, chorea, epileptic seizures, migraine with or without aura, psychosis, transverse myelopathy, Devic’s syndrome, and multiple sclerosis-like presentations.5 Cerebrovascular disease, one of the most common presenting symptoms of APS, accounts for half of the neurological manifestations in patients with APS.6
Levine et al. reported two cases of cerebral venous and dural sinus thrombosis associated with antiphospholipid antibodies.7 Similarly, Mortifee et al. reported communicating hydrocephalus in SLE with antiphospolipid antibody syndrome (secondary APS) in a 24-year-old woman.5 Wani et al. reported a case of primary antiphospholipid syndrome presented with lower cranial nerve palsy, aseptic meningitis, and hydrocephalus.2 The current study is presenting a case of gross communicating hydrocephalus without any focal neurological signs, except for secondary optic atrophy due to raised intracranial pressure. We ruled out tuberculosis and other infections on the basis of various CSF analyses. Although, Behcet’s disease is a cause of cerebral venous thrombosis, the disease occurrence was ruled out due to the absence of other markers of Behcet’s such as recurrent oral ulcers or other skin lesions.
Key message
Though CNS involvement has been recognized widely in patients with primary APS, hydrocephalus in APS may be seen only rarely.
Radiological modalities such as CT, MR or MRV can be helpful in demonstrating hydrocephalus, detecting the type of hydrocephalus, differentiating from other neurological involvement patterns, and to understand the main cause of hydrocephalus (such as dural sinus thrombosis, post inflammatory lesion of CNS lupus, cortical-deep venous structure damage, etc.).
It could be inferred that unusual presentations of primary APS, as in the present case, need to be considered for timely diagnosis and management.
Competing interests
The authors declare that they have no competing interests.
References
1. Mortifee PR, Bebb RA, Stein H. Communicating hydrocephalus in systemic lupus erythematosus with antiphospholipid antibody syndrome. J Rheumatol. 1992 Aug;19(8):1299-302.
2. Wani AM, Hussain WM, Fatani MI, Qadmani A, Maimani GAA, Turkistani A, et al. Lower cranial nerve palsy, aseptic meningitis and hydrocephalus: unusual presentation of primary antiphospholipid syndrome. BMJ Case Rep. 2009;2009.
3. Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J. Thromb. Haemost. 2006 Feb;4(2):295–306.
4. Hughes GR. Thrombosis, abortion, cerebral disease and the lupus anticoagulant. BMJ 1983;287:1088-9.
5. Tanne D, Hassin-Baer S. Neurologic Manifestations of the Antiphospholipid Syndrome. Curr Rheumatol Rep. 2001 Aug;3(4):286-92.
6. Sastre-Garriga J, Montalban X. APS and the brain. Lupus 2003;12(12):877-82.
7. Levine, S.R., Kieran, S, Puzio K, Feit H, Patel SC, Welch KM. Cerebral venous thrombosis with lupus anticoagulant. Report of two cases. Stroke. 18, 1987 Aug;18(4):801-4.