Original Articles
Clinical and immunogenetic characteristics of psoriatic arthritis: a single-center experience from South India
Mithun CB1, Paul T Antony2, Christina M Mariaselvam3, Vir S Negi4 *
Author Affiliations
1, 2, 3, 4Dept. of Clinical Immunology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India
*Correspondence: Dr. V S Negi, Professor and Head, Dept of Clinical Immunology, JIPMER, Pondicherry, India
IJRCI. 2013;1(1):OA1
Received: 13 December 2012, Accepted: 30 January 2013, Published: 26 February 2013
© IJRCI
Abstract
Aim
The aim of this study was to determine the clinical characteristics and prevalence of HLA B27 in patients with psoriatic arthritis presenting to a tertiary care centre in South India.
Background
Although the prevalence of psoriasis is high in India, there is paucity of data, especially on Ps A.
Materials and methods
This retrospective study included 141 patients satisfying the ClASsification criteria for Ps A (CASPAR). Demographic, clinical, and laboratory data of the patients were collected through personal interviews, clinical examination, appropriate investigations, and analysis of case records. HLA-B27 typing by PCR method was done for all patients.
Results
Among the 141 patients, 89 subjects were males and 52 were females, and the male to female ratio was 1.7:1. Polyarthritis (n=51, 36.2%) was the most common Ps A subtype noted during the study, followed by oligoarthritis (n=48, 34%), spondyloarthropathy (n=29, 20.6%), distal interphalangeal (DIP) predominant arthritis (n=25, 7.8%), and arthritis mutilans (n=2, 1.4%). Arthritis preceded skin involvement in 9.2% (n=13) of the cases. Dactylitis was seen in 24.1% (n=34) of the patients. Extra-articular features like enthesitis (n=16, 11.3%) and eye involvement (n=1, 0.7%) were also observed. Deformities were seen in 32.6% (n=46) of the subjects. The most common type of psoriatic skin lesion noted was psoriasis vulgaris (n=119, 84.4%). Nail involvement was seen in 17.7% (n=25) of the patients and it was observed in all subjects with DIP predominant arthritis (100%). Family history of psoriasis was present in 11.3% (n=16) of the patients. The number of patients positive for HLA B27 was 16 (11.3%). Additionally, the antigen positivity was noted in 35.7% (n=10) of the patients with spondyloarthropathy.
Conclusion
Ps A was more common in males. Polyarthritis and oligoarthritis were the most prevalent subtypes. The prevalence of HLA-B27 in our study population was 11.3% and was found to be strongly associated with spondyloarthropathy.
Introduction
Ps A is a chronic inflammatory disease with a broad spectrum of clinical features like dactylitis, enthesitis, inflammatory low backache, nail involvement, and eye manifestations like anterior uveitis and conjunctivitis. In 1973, Moll and Wright classified Ps A into five subtypes: 1. Distal interphalangeal (DIP) arthritis alone 2. Arthritis mutilans (destructive) 3. Symmetric polyarthritis. 4. Asymmetric oligoarthritis and 5. Spondyloarthropathy.1 The CASPAR group defined this classification more precisely: DIP predominant defined as more than 50% of total joint count being DIP joints; polyarthritis as ≥ five joints involved; oligoarthritis as <five joints involved; arthritis mutilans as destructive form of arthritis associated with flail joints; and spine predominant Ps A as inflammatory spinal pain, reduced spinal movements, and radiographic sacroiliitis.2 As per the definition, the term ‘symmetric’ is no longer used in conjunction with polyarthritis. Previous studies indicate oligoarthritis as the most common subgroup, whereas more recent findings suggest polyarticular variety as the most prevalent subtype.
There is a paucity of clinical data from India on Ps A. In this study, we have analyzed the clinical characteristics and their association with HLA-B27 status in Ps A patients attending a tertiary care center in South India.
Materials and methods
This retrospective study analyzed the demographic, clinical, and laboratory data of all patients with Ps A who had attended the clinical immunology department of a large tertiary care hospital between January 2009 and August 2012. We screened 157 patients who were previously diagnosed as Ps A based on treating physician’s opinion, and only those meeting the CASPAR criteria were included in the study.3 The data was collected through personal interviews, clinical examination, appropriate investigations, and analysis of case records. The patients were classified into different subtypes according to the CASPAR modification of Moll and Wright’s criteria.2 Appropriate X-rays were taken in all cases. Nephelometric measurement of rheumatoid factor and HLA-B27 typing by PCR were performed in all patients. The association of Ps A subgroups and different types of psoriatic skin lesions with HLA-B27 was analyzed by odds ratio (OR) and corresponding 95% confidence interval (CI). Statistical analysis was carried out using the Compare 2 software version 1.02.
Results
One hundred and forty-one patients fulfilling the CASPAR criteria were included in our analysis. Sixteen patients were excluded as they did not satisfy the CASPAR criteria. The corresponding number of male and female subjects considered was 89 and 52, with a male to female ratio of 1.7:1. Most of the study participants were in the fourth and fifth decades of life.
Polyarthritis (36.2%) was the most common subtype of Ps A seen in study subjects, followed by oligoarthritis (34%), spondyloarthropathy (20.6%), DIP predominant arthritis (7.8%), and arthritis mutilans (1.4%). DIP joint involvement was seen in 25 patients (17.4%). Among the 29 patients, who were classified into the spondyloarthritis group, six (20.7%) had isolated axial involvement. The two patients diagnosed with arthritis mutilans were above the age of 60 years. Although the number of patients with oligoarthritis was higher in the fourth decade (not statistically significant), the pattern of presentation was similar in all age groups except arthritis mutilans (Figure 1).
Figure 1: Age distribution and pattern of presentation of psoriatic arthritis
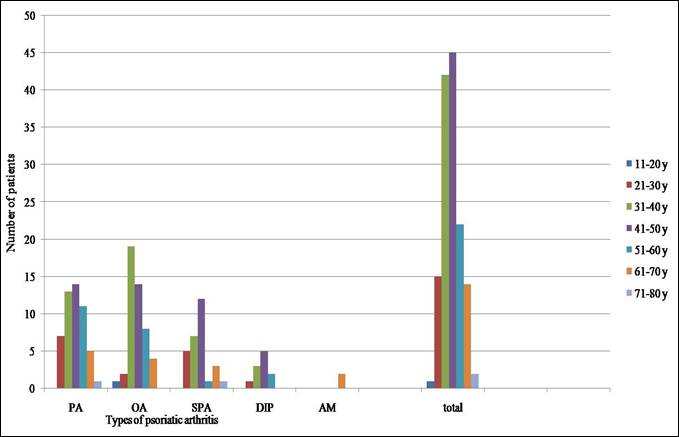
PA- Polyarticular, OA- Oligoarticuar, SPA- Spondyloarthritis, DIP- Distal interphalangeal joint predominant arthritis, AM- Arthritis mutilans
Out of 141 patients, deformities of joints were seen in 46 subjects (32.6%). Dactylitis and enthesitis were noted in 24.1% and 11.3% of the patients respectively. Eye involvement in the form of episcleritis was seen only in one patient (Table 1).
Psoriasis vulgaris was identified as the most common type of psoriatic skin lesion (84.4%). Isolated scalp psoriasis (5%) and flexural psoriasis (3.5%) were the other commonest groups. Typical psoriatic nail changes were observed in 17.7% of the subjects. Isolated nail involvement without skin involvement was seen in two patients (2.1%). All the patients with DIP predominant arthritis had nail involvement. Arthritis preceded skin involvement in 13 (9.2%) cases. Family history of psoriasis was present in 16 (11.3%) patients (Table 1).
Table 1: Demographic and clinical features of subjects
|
Total number of patients |
141 |
||
|
M:F |
1.7:1 |
||
|
Variables |
Number (Percentage) |
||
|
Subtypes of psoriatic arthritis [cumulative pattern] |
Polyarthritis |
51 (36.2%) |
|
|
Oligoarthritis |
48 (34%) |
||
|
Spondyloarthropathy |
29 (20.6%) |
||
|
DIP predominant |
25 (17.7%) |
||
|
Arthritis mutilans |
2 (1.4%) |
||
|
Deformities |
46 (32.6%) |
||
|
Dactylitis |
34 (24.1%) |
||
|
Enthesitis |
16 (11.34%) |
||
|
Eye involvement |
1 (0.7%) |
||
|
Psoriasis types |
Psoriasis vulgaris |
119 (84.4%) |
|
|
Scalp psoriasis |
7 (5%) |
||
|
Flexural psoriasis |
5 (3.5%) |
||
|
Palmoplantar psoriasis |
4 (2.8%) |
||
|
Erythroderma |
2 (1.4%) |
||
|
Pustular psoriasis |
1 (0.7%) |
||
|
Only nail involvement |
3 (2.1%) |
||
|
Overall nail involvement |
25 (17.7%) |
||
|
Arthritis preceding psoriasis |
13 (9.2%) |
||
|
Family history of psoriasis |
16 (11.3%) |
||
|
HLA-B27 positivity |
16 (11.3%) |
||
The results of HLA-B27 typing were available for 139 patients. The study findings reported 16 patients (11.3%) as positive for HLA-B27. Among these, 10 patients (62.5%) belonged to the spondyloarthropathy group. Out of the remaining six patients, four had oligoarthritis (25%) and two had polyarthritis (12.5%). In the spondyloarthropathy group, HLA-B27 was positive for 35.7% of the patients. Statistical analysis demonstrated that HLA-B27 positivity was strongly associated with spondyloarthropathy group (OR=9.72; 95% CI=2.739 to 36.055; P=0.000). Fifteen out of sixteen HLA-B27-positive patients had psoriasis vulgaris (OR=2.74; 95% CI=0.374 to 121.351; P=0.544). The number of HLA-B27-positive patients noted in different psoriatic arthritis subtypes is listed in table 2.
Table 2: Distribution of HLA-B27 among different psoriatic arthritis subtypes
|
Ps A subtypes
|
Number of HLA-B27- positive patients (n) (%) |
Number of HLA-B27- negative patients (n) (%) |
Odds ratio (OR) |
Confidence interval (CI) |
P value |
|
Spondyloarthropathy |
10 (35.7) |
18 (64.3) |
9.72 |
2.74-36.06 |
0.000 |
|
Oligoarthritis |
4 (8.3) |
44 (91.7) |
0.60 |
0.13-2.14 |
0.567 |
|
Polyarthritis |
2 (3.9) |
49 (96.1) |
0.22 |
0.02-1.01 |
0.063 |
Discussion
The demographic and clinical characteristics of Ps A could be influenced by different factors including genetic and environmental, and the diverse diagnostic criteria used in studies. In contrast to majority of the studies that showed an equal sex predisposition for psoriatic arthritis, the present study showed that the prevalence is more in a male-predominant population.5, 6, 9, 11, 12 Certain studies from India (Rajendran et al. and Prasad et al.) have also reported a male predisposition.7,13 Similar to the age pattern of patients in other studies, majority of our study participants were in the fourth and fifth decades of life.3, 7, 13 The prevalence of arthritis mutilans was more in the older age group (seventh decade). A recent study by Rodriguez-Moreno et al. also reported analogous findings.14 Similar to other studies, the occurrence of skin lesions preceded arthritis in majority of the cases. Arthritis preceded skin lesions in 9.2% of the study subjects. Evidence from previous studies also shows that arthritis can occur before skin lesions in 6 to 18%.5, 6, 7, 8, 11, 12, 15
We followed CASPAR modification of Moll and Wright proposal for subgrouping psoriatic arthritis.2 This modification by CASPAR defines psoriatic arthritis subgroups more precisely when compared to the original classification by Moll and Wright.1 The most prevalent clinical subtype observed during our study was polyarthritis and the subsequent order of prevalence of subtypes noted was; oligoarthritis, spondyloarthropathy, DIP predominant arthritis, and arthritis mutilans. These findings are largely in agreement with other studies; although there is a wide variation in the proportion of psoriatic spondyloarthropathy patients (Table 3). The difference in figures for psoriatic spondyloarthropathy may be due to the absence of well-defined classification criteria for the disease or difference in the genetic background of the study groups.
Table 3: Comparison of distribution of subtypes of psoriatic arthritis [cumulative pattern] with previous studies
|
Study |
Country |
Year |
n |
Polyarthritis (%) |
Oligoarthritis (%) |
Spondylitis (%) |
DIP (%) |
Mutilans (%) |
|
Present study |
India |
2013 |
141 |
36.2 |
34 |
20.6 |
7.8 |
1.4 |
|
Roberts et al.4 |
UK |
1976 |
168 |
79.8 |
16.8 |
4.9 |
NA |
NA |
|
Torre Alonso et al.5 |
Spain |
1991 |
180 |
35.6 |
37.2 |
22.8 |
NA |
4.4 |
|
Jones et al.6 |
UK |
1994 |
100 |
63 |
26 |
6 |
1 |
4 |
|
Rajendran et al.7 |
India |
2003 |
116 |
48.3 |
37.1 |
11.2 |
2.6 |
0.9 |
|
Michet et al.8 |
USA |
2005 |
504 |
65 |
NA |
18.6 |
NA |
NA |
|
Madland et al.9 |
Norway |
2005 |
634 |
68.6 |
28.7 |
2.7 |
0 |
0.6 |
|
CASPAR et al.3 |
Multiple countries |
2006 |
588 |
63 |
13 |
14 |
4 |
3 |
|
Reich et al.10 |
Germany |
2009 |
312 |
58.7 |
31.6 |
NA |
NA |
4.9 |
|
Zisman et al.11 |
Israel |
2012 |
149 |
49.7 |
34.2 |
17.5 |
19.5 |
3.3 |
Similar to the study findings by Simon et al. and Siannis et al., we have also reported the presence of deforming disease in 32.6% of the patients.16, 17 In contrast, another study from India by Rajendran et al. showed a lesser prevalence of deformities.7 Since, we have not examined the treatment effect and disease duration, it is difficult to comment about the factors associated with the deforming disease. However, the increased prevalence of deformities noted in our study confirms the fact that Ps A is not a benign disease. The prevalence of dactylitis and enthesitis reported were similar to the observations of Rajendran et al., whereas other studies showed a higher prevalence.3, 7, 8, 11, 18, 19 Akin to studies from Asia, eye involvement was very rare in present study.7, 20
In concurrence with the available literature, the current study also reports psoriasis vulgaris as the most common type of skin lesion observed (Table 4). Flexural and scalp psoriasis forms the second commonest disease, thereby highlighting the importance of examining the hidden sites like scalp and flexures for psoriatic skin lesions.
Table 4: Comparison of demographic features and skin involvement in psoriatic arthritis with previous studies
|
Study |
M:F |
Arthritis preceding psoriasis (%) |
Psoriasis type (%) |
Only nail involvement (%) |
|
Present study |
1.7:1 |
9.2 |
V84.4, G0, E1.4, P0.7, PP2.8, F3.5, S5 |
1.5 |
|
Gladman et al.12 |
0.9:1 |
17 |
V94, G 4 |
2 |
|
Jones et al.6 |
0.8:1 |
18 |
V89, G4, P3 |
0 |
|
Rajendran et al.7 |
2.1:1 |
12.1 |
V81, G1, E9, P4 |
4.3 |
|
Prasad et al.13 |
5.6:1 |
0 |
V72.5, G5, E2.5, P15 |
0 |
|
Torre Alonso et al.5 |
1.2:1 |
14.9 |
V94, G1, E3, P2 |
2 |
|
Zisman et al.11 |
0.8:1 |
9.9 |
NA |
NA |
|
Madland et al.9 |
1.1:1 |
NA |
V94, P6 |
NA |
|
Michet et al.8 |
1.4:1 |
6 |
NA |
NA |
|
Noosent and Gran15 |
1.4:1 |
13.8 |
NA |
NA |
V- Vulgaris, G- Guttate, E- Erythrodermic, P- Pustular, PP- Palmoplantar, F-Flexural, S- Scalp alone
The prevalence of HLA-B27 in our study population (11.3%) was slightly less when compared to the earlier reported prevalence ranging from 19 to 30%.21, 22, 23, 24, 27 It is interesting to note that no other studies have been reported from India on the prevalence of HLA-B27 in psoriatic arthritis. Based on the available evidence, it could be concluded that HLA-B27 is strongly associated with spondyloarthropathy.22, 24, 25, 26, 27 But, the prevalence of HLA-B27 in psoriatic spondyloarthritis was found to be much lesser than that in ankylosing spondylitis (prevalence of the antigen was more than 90).28 This could be due to the distinct genetic characteristics of psoriatic arthritis. In addition to HLA-B27, other HLA- genes play a significant role in Ps A susceptibility; whereas in ankylosing spondylitis, HLA-B27 is the major susceptibility gene.
Previous studies have showed an association between palmoplantar pustulosis and HLA-B27 positivity.23, 29 However, in our study we could not find any significant association between psoriatic skin lesions and HLA-B27 positivity.
To the best of our knowledge, this is one of the largest Ps A study series from India and the first one from the country showing the prevalence of HLA-B27 in psoriatic arthritis. Most of the clinical characteristics of Ps A reported in our study comply with the studies from other parts of the world. However, extra-articular features were less prevalent in the present study.
Authors’ contributions
Mithun CB, Paul T Antony, and Vir S Negi conceived and planned the study; Christina M Mariaselvam carried out immunological and molecular diagnostics; Mithun CB, Paul Antony, Christina M Mariaselvam, and Vir S Negi contributed equally to data analysis and manuscript preparation.
Competing interests
The authors declare that they have no competing interests.
References
1. Moll JMH, Wright V. Psoriatic arthritis. Semin Arthritis Rheum. 1973;3:55-78.
2. Helliwell PS, Porter G, Taylor WJ, CASPAR Study Group. Polyarticular psoriatic arthritis is more like oligoarticular psoriatic arthritis, than rheumatoid arthritis. Ann Rheum Dis. 2007;66:113-117.
3. Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H,et al. Classification criteria for psoriatic arthritis: Development of new criteria from a large international study. Arthritis & Rheumatism. 2006; 54(8): 2665-2673.
4. Roberts MET, Wright V, Hill AGS, Mehra AC. Psoriatic arthritis: follow up study. Ann Rheum Dis. 1976;35:206-212.
5. Torre Alonso JC, Rodriguez Perez A, Arribas Castrillo JM, Ballina Garcia J, Riestra Noriega JL, Lopez Larrea C. Psoriatic arthritis: a clinical, immunological and radiological study of 180 patients. British J Rheumatol. 1991;30:245-250.
6. Jones SM, Armas JB, Cohen MG, Lovell CR, Evison G, McHugh NJ. Psoriatic arthritis: outcome of disease subsets and relationship of joint disease to nail and skin disease. Br J Rheumatol. 1994;33:834-839.
7. Rajendran CP, Ledge SG, Rani KP, Madhavan R. Psoriatic arthritis. J Assoc Physicians India. 2003; 51:1065-1068.
8. Michet CJ, Mason TG, Mazlumzadeh M. Hip joint disease in psoriatic arthritis: risk factors and natural history. Ann Rheum Dis. 2005; 64:1068-1070.
9. Madland TM, Apalset EM, Johannessen AE, Rossebö B, Brun JG. Prevalence, disease manifestations, and treatment of psoriatic arthritis in Western Norway. J Rheumatol. 2005; 32:1918-1922.
10. Reich K, Krüger K, Mössner R, Augustin M. Epidemiology and clinical pattern of psoriatic arthritis in Germany: a prospective interdisciplinary epidemiological study of 1511 patients with plaque type psoriasis. Br J Dermatol. 2009;160:1040-1047.
11. Zisman D, Eder L, Elias M, Laor A, Bitterman H, Rozenbaum M, et al. Clinical and demographic characteristics of patients with psoriatic arthritis in northern Israel. Rheumatol. 2012;32(3):595-600.
12. Gladman DD, Shuckett R, Russell ML, Thorne JC, Schachter RK. Psoriatic arthritis. An analysis of 220 patients. Q J Med. 1987;62:127-141.
13. Prasad PV, Bikku B, Kaviarasan PK, Senthilnathan A. A clinical study of psoriatic arthropathy. Indian Journal of Dermatology, Venereology and Leprology. 2007;73(3):166-70.
14. Rodriguez-Moreno J, Bonet M, Del Blanco-Barnusell J, Castaño C, Clavaguera T, Mateo-Soria L, et al. Mutilating/resorptive arthritis. a study of 24 patients in a series of 360 patients with psoriatic arthritis. Reumatol Clin. 2012 Dec 12 [Epub ahead of print]
15. Noosent JC, Gran JT. Epidemiological and clinical characteristics of psoriatic arthritis in northern Norway. Scand J Rheumatol. 2009;38:251-255.
16. Bond SJ, Farewell VT, Schentag CT, Gladman DD. Predictors for radiological damage in psoriatic arthritis: results from a single centre. Ann Rheum Dis. 2007; 66(3): 370-376.
17. Siannis F, Farewell VT, Cook RJ, Schentag CT, Gladman DD. Clinical and radiological damage in psoriatic arthritis. Ann Rheum Dis. 2006; 65(4): 478-481.
18. Brockbank JE, Stein M, Schentag CT, Gladman DD. Dactylitis in psoriatic arthritis: a marker for disease severity? Ann Rheum Dis. 2005 Feb;64(2):188-90.
19. Gladman DD, Chandran V. Observational cohort studies: lessons learnt from the University of Toronto Psoriatic Arthritis Program. Rheumatology (Oxford). 2011;50(1):25-31.
20. Thumboo J, Tham SN, Tay YK, Chee T, Mow B, Chia HP, et al. Patterns of psoriatic arthritis in orientals. J Rheumatol 1997;24:1949-53.
21. Eder L, Chandran V, Pellet F, Shanmugarajah S, Rosen CF, Bull SB, et al. Human leucocyte antigen risk alleles for psoriatic arthritis among patients with psoriasis. Ann Rheum Dis. 2012;71:50-55.
22. Queiro R, Torre JC, González S, López-Larrea C, Tinturé T, López-Lagunas I. HLA- antigens may influence the age of onset of psoriasis and psoriatic artritis. J Rheumatol. 2003;30:505-7.
23. Dalbeth N, Dockerty JL, Williamson L. Influence of HLA-B27 on the Clinical Presentation of Psoriatic Arthritis. J Rheumatol. 2003;30;2511.
24. Liao HT, Lin KC, Chang YT, Chen CH, Liang TH, Chen WS, et al. Human leukocyte antigen and clinical and demographic characteristics in psoriatic arthritis and psoriasis in Chinese patients. J Rheumatol. 2008; 35:891-5.
25. Chandran V, Tolusso DC, Cook RJ, Gladman DD. Risk Factors for Axial Inflammatory Arthritis in Patients with Psoriatic Arthritis. J Rheumatol. 2010;37;809-815.
26. Queiro R, Sarasqueta C, Belzunegui J, Gonzalez C, Figueroa M, Torre-Alonso JC. Psoriatic spondyloarthropathy: a comparative study between HLA-B27 positive and HLA-B27 negative disease. Semin Arthritis Rheum. 2002; 31: 413 -18.
27. Bonfiglioli R, Conde RA, Sampaio-Barros PD, Louzada-Junior P, Donadi EA, Bertolo MB. Frequency of HLA-B27 alleles in Brazilian patients with psoriatic arthritis. Clin Rheumatol. 2008; 27: 709- 12.
28. Brown MA. Genetics of ankylosing spondylitis. Curr Opin Rheumatol. 2010 ; 22 : 126- 32.
29. Zachariae H, Overgaard Peterson H, Kissmeyer Nielson F, Lamm L. HLA- antigens in pustular psoriasis. Dermatologica. 1977;154:73-7.